Next month is open enrollment for University of Illinois health plans, and employees will have an opportunity to reevaluate which plan is best for them and their families. The goal is to strike a balance between managing out-of-pocket costs and optimizing financial benefits. How do you do that? We give you some factors to consider.
Annuities for Academics: TIAA Traditional Demystified
Disability Insurance: Covering the Underestimated Scenario
Regardless of your employer, remember that it is all too common to underestimate the possibility of an extended illness or other event that would make full-time employment impossible. Take a closer look at the disability benefits offered through your employer and consider if additional long-term disability insurance would protect the financial health of your family.
Navigating Benefit Decisions during the University of Illinois Urbana-Champaign’s Open Enrollment
Making Sense of Medicare IRMAA, a Universally Confusing Topic
The forename Irma is of Germanic origins and means “universe.” For many retirees, Medicare IRMAA is of universally confusing origin. In this article we’ll cut through some of the bewilderment, and hopefully leave you with a sounder understanding of IRMAA’s purpose, calculation, and planning opportunities.
Retiree Health Insurance Under SURS
Introduction
We have found that retiree health insurance benefits can be the most common point of confusion for State of Illinois employees retiring under the State University Retirement System (SURS). In this post, we will break down the basics of the Retiree Health Insurance Benefit, how to qualify, and the features and drawbacks of this benefit.
Special Note for SURS Retirement Savings Plan participants: In fall of 2020, SURS rolled out the newly rebranded SURS Retirement Savings Plan (RSP), which has added another layer of complexity. See the whitepaper we wrote for a more detailed overview of this change.
Qualifications
Service Credit
To begin, let’s discuss the qualifications for retiree health insurance benefits. The first requirement is service credit. Service credit can vary based on your SURS membership Tier, which is determined by the date of first employment under a SURS covered employer. For anyone with service credit prior to January 1, 2011, you are considered a Tier I participant. A Tier I participant is eligible for retiree insurance benefits after 5 years of service credit. Anyone beginning service credit on or after January 1, 2011 is a Tier II participant. 10 years of service credit is required for Tier II participants to be eligible for any retiree health insurance benefit.
The service credit discussed above is the minimum requirements to be eligible for retiree health insurance. Meeting the minimum service credit requirements only provides for a subsidy of the cost of this benefit. To have your insurance fully subsidized by the State of Illinois, you need 20 years of service credit. Members who meet the minimum coverage requirements and have less than 20 years split the cost of coverage with the state. The chart below summarizes this cost split:
Costs above are for the employee only. Coverage for a spouse or dependents is available for an additional cost.
Annuity Election
The second requirement in addition to meeting the service credit requirements to qualify for retiree health insurance is to annuitize your pension. If you separate from service and defer taking a monthly retirement benefit under SURS, you would not be entitled to the retiree insurance benefit until you have annuitized your pension plan. Taking a refund of your pension plan balance, including rolling over your plan balance to an IRA or other retirement plan will result in a forfeiture of retiree health insurance benefits.
Annuitization of SURS is the process of converting your benefit into a stream of income payable monthly for the remainder of your life. For the Traditional and Portable plan, this is fairly straightforward. Your pension is based the higher of two formulas which SURS will calculate for you. Your main decision is whether to select a survivor benefit for your spouse or a qualified dependent.
The Retirement Savings Plan has more flexibility, which makes annuitizing a bit more complex. Here is a summary of your options.
1. Annuitize the entire balance of your SURS RSP. This annuity will generally be administered for SURS through Principal Insurance company, or at TIAA if you still have funds in your RSP portfolio invested at TIAA.
2. Move at least 50% of your RSP portfolio balance into the SURS Secure Income Portfolio and activate the lifetime income benefit. When selecting this option, all RSP investment funds not otherwise annuitized must be first moved into the Lifetime Income Strategy (LIS) portfolio. Next, with all non-annuitized RSP funds in the LIS portfolio, at least 50% of those LIS funds must then be moved into the SIP with its guaranteed income benefit. After moving all funds into the LIS and activation of at least 50% of your LIS fund total into the guaranteed SIP, any LIS funds not in the SIP may be moved back to RSP Core Funds or withdrawn.
3. A combination of Options 1 & 2 – for example, you could use 1/3rd of your RSP account to buy an annuity through Principal. With the remaining RSP balance, allocate 50% to the SIP for lifetime income and 50% to the LIS or Core Funds for periodic withdrawal.
We have commonly heard the misconception that RSP participants must use the new SIP to maintain health insurance, which is not true. Electing an annuity remains an option.
Timing of Retiree Health Insurance
It is possible to retire from the University and delay drawing your pension. This may be beneficial if you have alternative insurance coverage through new employment or a spouse. Deferring your benefit has two potential benefits. First of all, your pension benefit (traditional or portable) may increase or the balance of your account can continue to grow (RSP). Secondly, if you are not yet Medicare-eligible, the State of Illinois will pay an additional monthly incentive to opt out of retiree insurance.
Example 1
A University Employee has 20 years of service at age 50, at which point she leaves university employment to pursue a second career with a private sector employer. The new employer offers health insurance. The employee leaves her account balance with the SURS RSP, which allows the balance to continue to grow. At age 63, she fully retires from her private sector position and needs health insurance. At this point, she activates one of the RSP income options to qualify for health insurance as a State of Illinois retiree.
The Value of Retiree Health Insurance under SURS
There may be cases where an individual chooses to forgo their SURS retiree health insurance benefits, but before making this irrevocable decision, it is important to understand what those health insurance benefits are worth.
How SURS Retiree Health Insurance works with Medicare
Those in the SURS RSP are also required to participate in Medicare. While working, everyone pays into the Medicare system. Upon turning age 65, you must sign up for Medicare. If you are still working and covered by your University insurance, you only need to enroll in Medicare Part A, but may delay Part B until you retire.
Medicare has three parts:
Part A, which covers Hospital services and is generally free for those age 65+
Part B, which covers doctor visits and other outpatient services. Part B has a monthly premium starting at $170.10 (2022); cost can increase based on income.
Part D, which covers prescription drug costs
Once you retire and become a SURS annuitant aged 65 or older, you are required to enroll in the Total Retiree Advantage Illinois (TRAIL) plan, managed through Illinois Central Management Services (CMS). This is a Medicare Advantage plan, which means it combines Medicare Part A, Part B, Part D and a Medicare Supplemental Policy (commonly known as a Medigap policy). Even under the TRAIL program, you still must pay the Medicare Part B premiums on your own. The State of Illinois subsidizes (or entirely covers) the rest of your supplemental health cost.
How much is this SURS health insurance subsidy worth?
For a retiree with 20 or more years of service, age 65 or older and on Medicare, the value of this benefit is around $150 per month. This is based on the amount the State of Illinois covers for the cost of the Advantage Plan (Illinois Central Management Services, 2022).
For a retiree with 20 or more years of service and under the age of 65, the SURS health insurance benefit is significantly more valuable. Prior to Medicare eligibility, the State picks up the entire cost of their health insurance. For those retiring before age 65, the cost of health insurance can be a significant obstacle. For example, marketplace plans at healthcare.gov range in cost from $1,165 to $1,791 for a 60 year old male in the Champaign County area.
Conclusion
Health Insurance is one of the biggest obstacles we see for clients who wish to retire prior to eligibility for Medicare at age 65. If you are retiring early from the University, it could be a valuable benefit. The requirement to annuitize is the biggest obstacle, especially for those in the SURS Retirement Savings Plan. Once you are Medicare eligible, the value of the insurance benefit is less valuable as Medicare covers a significant portion medical expenses and Medicare supplement policies are low in cost as compared to private health insurance.
Update on Illinois Retiree Insurance
We have heard from many of our clients regarding concerns over the change in Insurance Providers for State of Illinois Medicare-Eligible Retirees. With so many clients impacted by this change, we have been following the news. Here is what we know so far and what we are recommending.
Starting with what we know, it is not much. We wrote up a short piece on our website on this a few weeks back, which you can read here. The major concern at this time is that Carle has not come to an agreement with the Advantage Plan Provider, Aetna. This means that Carle providers and facilities are not in-network for the new plan effective January 1, 2023. While the new plan is a PPO and should allow you to see out-of-network doctors, these services may not be covered if the provider is unwilling to bill through Aetna.
As far as we can tell, conversations between Carle and Aetna are ongoing and there is a possibility that an agreement will be reached before the new plan year. This would not be unprecedented. A similar process unfolded about 10 years ago when Health Alliance was dropped in favor of UnitedHealthcare. Recent comments from Carle and Aetna representatives may be more attempts to rally public pressure for negotiations than statements of actual status of negotiations.
The unfortunate part is this leaves a lot of uncertainty for current plan participants. Here is what we are recommending:
If you are currently undergoing treatment for chronic or critical medical issues and absolutely cannot switch doctors, be prepared to switch to a private policy:
November 30th – Deadline to opt out of the TRAIL / State of Illinois Medicare Plan
December 7th – Deadline for Medicare Open Enrollment to select your own private plan
Research Alternative Plans - Medicare's Website is the best resource as you can narrow in to providers covered in your area.
Private policies generally run $50-175/month/person, but can be higher or lower depending on deductible, co-pays, etc.
Inputting your current prescriptions will provide you a better total out of pocket cost estimate.
Pay attention to vision and dental coverage.
For everyone else, it is probably best to take a wait-and-see approach. If Carle and Aetna reach an eleventh hour agreement, you avoid all the hassle of unenrolling and reenrolling from TRAIL next year. If they do not reach an agreement, you could also unenroll from TRAIL during the next enrollment period near the end of 2023.
INSURANCE CHANGES FOR ILLINOIS STATE RETIREE HEALTH INSURANCE
In September, the State of Illinois Department of Central Management Services (CMS) announced changes to the State of Illinois Retiree Insurance Program. These changes impact retirees enrolled in the Total Retiree Advantage Illinois (TRAIL) who are also Medicare Eligible. This applies to members who are currently enrolled, or plan to enroll in the TRAIL Medicare Advantage Prescription Drug (MAPD) plan effective for the 2023 plan year.
Following a proposal process, the State of Illinois has selected Aetna Medicare Advantage Prescription Drug (MAPD) PPO Plan as the new medical and prescription drug plan beginning January 1, 2023. This will replace the existing plans, most commonly the HMO Plans through UnitedHealthcare, Health Alliance, or Humana. This change is automatic and does not require participants to take any action .
Here are a few Frequently Asked Questions (FAQs) that may help you:
Why is this change happening?
The contract with current providers expires December 31, 2022. State law requires a competitive process to compare proposals submitted by various vendors. Aetna was selected as part of this process.
With any change in insurance provider also comes concern over coverage of existing doctors and hospitals. While it is yet to be seen how these concerns will be addressed, it is worth noting this is not a new process. A similar process unfolded when Health Alliance was dropped in exchange for UnitedHealthcare.
Can I maintain my current Medicare Advantage Plan Provider?
No. To maintain coverage under the Total Retiree Advantage Illinois (TRAIL), including subsidized premiums under your retirement annuity, you and your dependents will automatically change to the new provider.
You may opt of out of TRAIL by visiting MyBenefits.illinois.gov. This must be completed by November 30, 2022. If you opt out, you will want to select a new Medicare Supplement and Part D or Medicare Advantage plan in the private market. You will be responsible for the full premiums for these Supplement/Advantage plans. You can compare plans at Medicare's Website. If you opt out, you may re-enroll in the TRAIL program with a qualified life event or during the next year’s open enrollment.
What if I am not Medicare Eligible?
This change only impacts members and their dependents whose coverage is under a Medicare Advantage plan. If you or any dependents are not Medicare-eligible, your coverage is through the State Employees Group Insurance Program (SEGIP) and is not impacted by this change. This change may impact you if you become Medicare eligible in the future.
What is a Medicare Advantage Plan?
Medicare is commonly made up of three parts:
Part A – Covers Hospital Services
Part B – Medical Insurance
Part D – Prescription Drugs
Most Medicare participants also add a Medicare Supplement plan to cover any gaps and add services above the base Medicare plans.
Medicare Advantage Plans combine all the above plans into a single plan, administered through a private health insurance company. In this case, Aetna is the private company who will take over administration.
Do I pay Medicare Premiums if I am enrolled in a Medicare Advantage Plan?
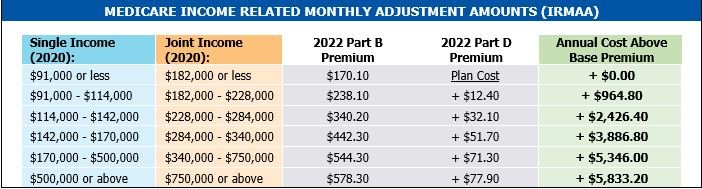
Yes. While a Medicare Advantage plan replaces original Medicare, you are still responsible for Medicare Part B premiums, which are either paid directly to Medicare or deducted from Social Security benefits. Note that, for most people, Medicare Part A is free (paid through Payroll taxes while working). Your Part B premium is based on your income and can change from year to year. Part D may also have a supplemental cost. These premium adjustments are called the Income Related Monthly Adjustment Amounts (IRMAA) as follows:
What’s Next for Me?
As mentioned previously, for those opting out, actions will need to be taken. For those choosing to stay on the TRAIL MAPD program, the change is automatic for members and their dependents. You will receive a welcome kit in the mail from Aetna with more information on the plan and new member ID Cards. With all the Medicare spam mail that gets sent out, keep a sharp eye out for any correspondence from AETNA, CMS, or anything with the TRAIL logo.
Further Reading and Sources:
SURS News Release Retiree Healthcare Update - SURS
Illinois Central Management Services My Benefits Website
Aetna Coverage Details State of Illinois | Aetna Medicare
Medicare Premiums Detail at Social Security - IRMAA Sliding Scale Tables
TRAIL Enrollment Guide (2022) FY 2022 Benefit Choice
Update on Illinois Pension Reform
For updated information on this subject please read our latest blog post. This year has seen a flurry of lawsuits related to Illinois Pension Reform, including previous changes made to the State Retiree Health Insurance. Many of the cases are still in process, but here is an update on what we know:
Pension Reform
In late 2013, Illinois General Assembly passed a bill aimed at reforming the pension systems for most Illinois public employees and Governor Pat Quinn signed the bill into law. This bill reduced future benefit increases for current retirees and decreased expected benefits for those not yet retired. Lawsuits quickly followed questioning the constitutionality of this law. The law was slated to go into effect as of June 1, 2014, but was suspended pending resolution of these lawsuits. This means that SURS and other State Retirement Systems are operating under the rules as they existed before pension reform was passed.
You can see my summary of the pension reform in two prior blog posts from December 6th and December 23rd. You can also view a SURS press release regarding the halting of pension reform here.
Health Insurance
Before the pension reform discussed above, changes were made in 2012 requiring State Retirees to contribute towards the cost of their health insurance by a 2% deduction from their pension (1% for retirees enrolled in Medicare). Like pension reform, lawsuits were filed challenging this law. The opinion of many experts at the time of passage was that Retiree Health insurance was a separate benefit from pension benefits and therefore not constitutionally guaranteed. This was further backed by an initial court ruling. Since that time, there has been more action by the courts.
First, the Illinois Supreme Court overturned the lower court's decision by ruling that Retiree Health insurance is in fact protected by the same constitutional provisions that protect pensions. Then, shortly after, another ruling halted the July 2014 planned increase in premium contributions to be made by pensioners. Finally, a ruling this week determined that the state may no longer deduct health insurance premiums from retirees' pensions.
You can read more about this change here.
Implications
It is still too early to make substantial planning decisions. Immediately, retirees can expect their pension benefit to increase in the next month or two as health care deductions are halted. It is also possible that previously deducted premiums will be refunded. For retirees who previously deducted premiums paid as an Medical Expenses under their Itemized Deductions on their tax returns, they may have to claim refunds as income.
Additionally, some retirees opted out of state insurance in favor of alternative Medicare Supplemental, Medicare Advantage or other policies. This might sway those retirees to return to the state plan during open enrollment for 2015.
Longer term the State's position on pension reform looks more weak, but this is a complex legal matter. I expect we are a long way from any final resolution.
Insurance changes for Illinois State Retiree Health Insurance
The following is information regarding recent changes to Illinois State Retiree Health Insurance. These changes only apply to those who are enrolled in Medicare. If you are affected by this change, you should be receiving a letter from CMS regarding the proposed changes to the SURS health insurance plan this week. Note: if you are covering a dependent, you must both be enrolled in Medicare for this change to affect you. If only one of you is enrolled in Medicare, then you will keep your existing coverage and May benefit choice period. Here is a summary of what we know:
Important! You must make a decision and enroll (postmarked) by December 13, 2013. There is no default choice. If you do not enroll, you will only have Medicare Parts A and B coverage which is very limited and does not include prescription drug coverage. New state coverage will start February 1st and run through December 31st of 2014. In future years, your open enrollment period for health insurance will be the same as the Medicare Fall enrollment period. You will note this has changed from May, as in past years, to fall enrollment for this year and future years. This is also the time to add or drop dependents, add, drop or change Optional life insurance coverage, and add or drop dental coverage.
Coverage Summary
Every county in the state has different choices of plan. Consult the map in the materials you receive, or follow this link and view page 8
In Champaign County, you have two choices of plans: UnitedHealthcare (UHC) PPO and Coventry Advantra HMO.
With the UHC plan, you can see any willing provider as long as the provider is in the Medicare program. You should note there is no difference for in-network and out-of-network coverage levels, as with most PPO plans. After a $100 deductible, you pay 10% of charges for services up to the $1,300 annual out-of-pocket maximum, then the plan covers 100%.
With the Coventry Advantra HMO plan, you must choose a primary care physician from within their network of providers, and use only in-network providers except for emergency care. There are copays, and the annual out-of-pocket maximum is $3000. There is a chart on page 11 of the Trail booklet comparing the costs for the two plans.
All SURS annuitants who are enrolled in Medicare Parts A&B (and SURS annuitants with Medicare enrolled dependents) will be required to enroll in a Medicare Advantage plan if they want to be covered by the SURS health insurance. These plans include prescription drug coverage (MA-PD plans; MA equals Medicare Advantage, including Part A and Part B coverage; PD equals Prescription Drug), so you do NOT have to enroll in a Medicare Part D plan.
Caution! Be careful when enrolling as you may also be receiving mailed offers from private Medigap insurance companies. These options do not qualify for State coverage. To enroll in the state plan, your forms must have the “Total Retiree Advantage Illinois” logo (Your TRAIL to Better Health). Here is the logo:
Vision, dental and life insurance benefit plans are not changing, but you must enroll in one of the State-sponsored plans to continue access to existing vision coverage. Life insurance and dental, if elected, continue automatically.
Carle Patients: It appears that if you want to stay with Carle doctors, you need to choose the UnitedHealthcare PPO.
The Coventry Advantra website will be available on November 1st. At that time, you can look there for their providers in Champaign County.
Other Notes:
For community college retirees, you are in the College Insurance Program (CIP); if your SURS is from a State University or State of Illinois Department, you are in the State Insurance Program. This is important, because prices are different for each program.
You could opt-out of state coverage and shop for an individual Medigap or Medicare Advantage coverage policy. You would lose any subsidy from SURS state coverage if you make this election. This could make sense if (1) premiums on a private policy are smaller than your 2014 2% of pension contribution (those with large pensions) or (2) you would rather pay a higher premium and continue on a Health Alliance Medicare plan.
If you are in the State Insurance program and you opt-out, you would have the option to enroll in the State-sponsored plan during the next open enrollment with coverage beginning January 2015.
If you are in the College Insurance program (CIP), opt-out provisions are different; you would want to verify them with CMS.
Complete information for: CIP – The Trail
Complete information for: State Insurance – The Trail
As always, please contact us if you have any questions or would like clarification.